Division of Global Emergency Medicine
Collaborating with international partners to expand the department's vision
The Mission of the Division of Global Emergency Medicine is to collaborate with international partners to extend the department's vision of discovering, teaching and delivering patient centered emergency care to low- and middle-income countries through the development of locally sustainable emergency medical systems.


Emergency Medicine development in Guyana
A sustainable partnership for education leads to the birth of a system.
Since Vanderbilt Emergency Medicine’s first visit to Guyana in late 2002, led by then-Chief Resident John Paul Rohde, who grew up in Georgetown in the 1980s, a robust Vanderbilt collaboration with the Guyanese public health sector and the Georgetown Public Hospital Corporation (GPHC) has made significant contributions to the development of Emergency Medicine in Guyana.
Changing the narrative of global health engagement
Shortsighted projects dependent on foreign resources
The modern history of global health engagement in low- and –middle-income countries by developed country institutions is marred by echoes of neocolonialism and harmful medical tourism.
However well intended, major philanthropists and governmental agencies have funded shortsighted and misguided projects that have commonly failed to result in sustainable local systems development and have often impaired lasting local progress by fostering dependency on foreign resources and by misaligning incentives.
By contrast, even as early as 2002, Vanderbilt’s initial conversations with GPHC’s then Director of Medical and Professional Services Dr. Madan Rambaran were infused with his vision of founding durable graduate medical education programs in all major specialties in Guyana as a key sustainable development objective.

A need for Guyanese physicians to return home
Prior to 2009, Guyanese physicians could obtain their initial medical degree either from the University of Guyana or in Cuba through an agreement between the Cuban and Guyanese governments, but no post-graduate residency training programs were locally available.
The post-graduate path to the practice of medicine was based on simply assigning junior doctors to a hospital department and putting them to work as informal apprentices to more experienced clinicians. To obtain bona fide specialty training, Guyanese physicians and surgeons had to leave the country to attend programs in the United States, Canada, Russia, Cuba, Great Britain, or the West Indies.
While some of these foreign trained specialists did return home and become medical leaders in Guyana, many were lost to the system because of the portability of foreign training and more attractive practice markets elsewhere.
A new DAWN, Project Donors and Workers Now
In 2009, Vanderbilt’s Division of Global Emergency Medicine became the grateful recipient of a grant from Project Donors and Workers Now (DAWN), a non-profit devoted to improving the health of the Guyanese people founded in 1985 by Dr. Carmen Gannon.
Also known as Sister Mary Carmen Gannon of the Sisters of Mercy, Dr. Gannon was an American Internal Medicine physician and nun, originally from Baltimore, who had developed a deep connection to the people of then British Guiana as she worked in the Mahaica Hospital as a nurse caring for patients with leprosy.
After completing her medical degree at George Washington and her residency at the Medical University of South Carolina in Charleston, she returned to Guyana and founded Project DAWN, leveraging international resources to provide locally unavailable surgical care for Guyanese patients.

Realizing the dream of sustainable graduate medical education
The Project DAWN gift allowed Vanderbilt to recruit Dr. Nicolas Forget, the first fellowship trained Global Emergency Medicine faculty member at Vanderbilt, who would eventually become known as the “Father of Emergency Medicine” in Guyana.
In 2010, shortly before Dr. Gannon’s death, Vanderbilt, the Georgetown Public Hospital, and the University of Guyana collaborated to launch the Master in Emergency Medicine residency program, the first degree-conferring residency program for physicians in the country.
Dr. Forget and his wife, Dr. Ruth Derkenne, a family physician and obstetrician who contributed monumentally to the local development of her own specialties, moved their family to live in Guyana for the three years it would take to get the residency program up and running.
In the decade that followed, this collaboration has become a sustainable partnership that has produced 27 fully trained emergency medicine physicians. The program has had 100% retention of Guyanese born graduates, with most graduates actively involved as educators in the residency program.
Dr. Zelda Luke-Blyden became the first local residency program director in 2018 and was succeeded in 2022 by Dr. SriDevi Jagjit. Drs. Luke-Blyden and Jagjit graduated in the class of 2015. Four graduates have returned to their home countries to become the first residency trained emergency medicine physicians in Grenada and Antigua.

The Georgetown Public Hospital and the University of Guyana, in collaboration with numerous international partners, now offer residency training programs in:
- Emergency Medicine
- General Surgery
- Orthopedics
- Internal Medicine
- Pediatrics
- Family Medicine
- Obstetrics and Gynecology
- Anesthesiology
- Radiology
- Psychiatry
Emergency Medicine Residency in Guyana has paid dividends, fostered progress
The Accident and Emergency Department at GPHC has been elevated to full department status within the institution and the residency program’s first graduate, Dr. Zulfikar Bux, serves as Head of Department and National Director of Emergency Medical Services.
With seed funding from the Morris Family Foundation, the National EMS Service launched in 2012. With 911-style public access, centralized dispatch, and online medical control by trained emergency physicians at GPHC, it has grown to over 80 basic EMTs in service and will add advanced EMT training early next year.
Alongside the Emergency Medicine residency program for physicians, Vanderbilt, GPHC, and the University of Guyana now offer a first-of-its-kind bachelor’s degree conferring two-year residency in Emergency Nursing lead by Vanderbilt’s Jessica VanMeter. With five classes and 42 graduates to date, it is revolutionizing emergency nursing care in Guyana.
Introduction of the American Heart Association life support courses (ACLS, BLS, PALS) and the creation of the GPHC’s own life support training center accredited by the Caribbean Heart Foundation.
Facilitation of a new and ongoing partnership between GPHC and Project DAWN which secured the use at cost of Project DAWN’s 30,000-square-foot facility near the University of Guyana for GPHC’s growing medical education needs. This facility houses the office of Guyana National Emergency Medical Services, accommodates visiting faculty, and serves as a training site. During the COVID-19 pandemic, it provided isolation housing for providers assigned to the COVID-19 specialty hospital at Ocean View.


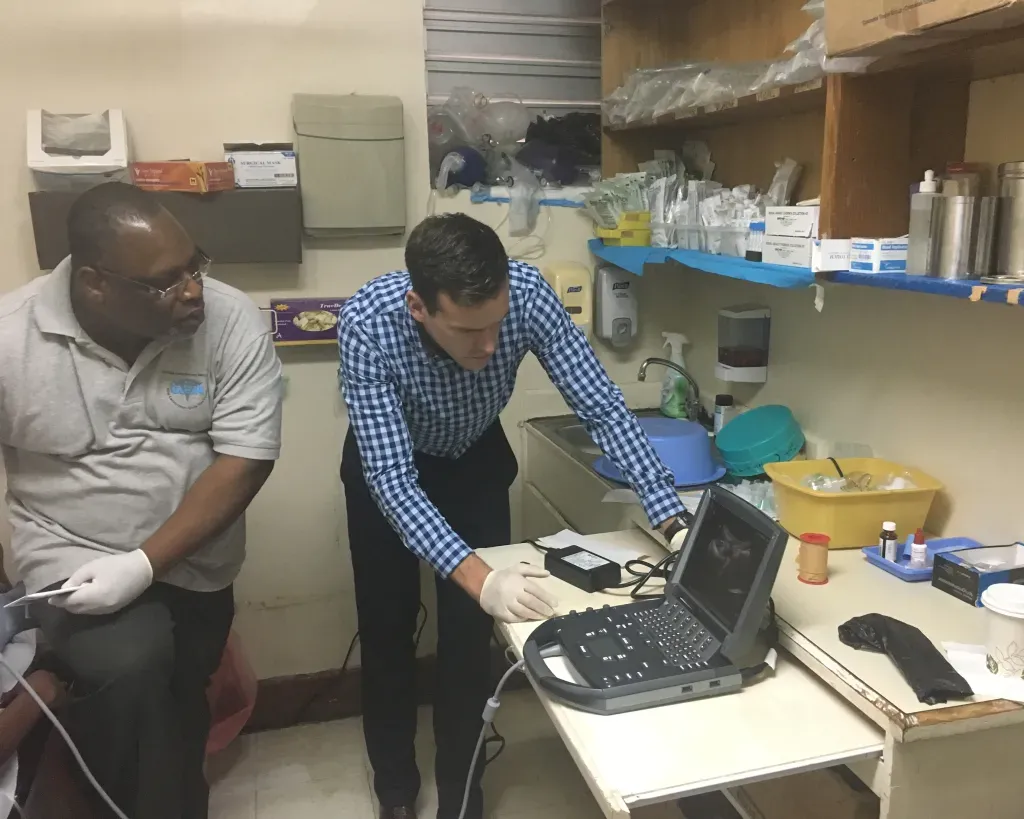
Development of additional specialized fellowship training programs for residency graduates in Emergency Ultrasonography and Emergency Department Administration, with future plans to add EMS, Simulation Education, Toxicology and Global Emergency Medicine.
Consultation by request of the GPHC board of directors on the redesign of the GPHC A&E Department by Vanderbilt chief architect Donald Blair, who donated his time and created a blueprint and recommendations for a new physical plant.
Creation of GPHC’s Trauma Registry database program, to collect epidemiologic data on accident and injury cases, to guide the future development of the program based on real data and patient outcomes.
When the COVID-19 pandemic struck Guyana, the government created an Infectious Diseases Specialty Hospital for COVID-19 patients and named a 2014 graduate of the GPHC EM residency, Dr. Tracey Bovell, to become its Chief Medical Officer based on her reputation as a leader in disaster preparedness.
We are deeply grateful to the many contributors who have dedicated their time and effort to advancing emergency medicine in Guyana

Thanks to their commitment, the specialty has become a reality in the country. With 27 graduates from the emergency medicine residency program and 100% retention of Guyanese-born graduates, leadership and education have successfully transitioned to local emergency medicine physicians.
While Vanderbilt continues to support the growth of emergency medicine in Guyana through initiatives such as expanding EMS to underserved regions, offering fellowship training opportunities for program graduates, and strengthening the local research platform, our Global Emergency Medicine division is actively forging new partnerships to support emergency medicine systems development and residency education in other international locations.
Our hope is to incorporate many of our Guyanese graduates into these new partnerships, truly expanding the reach and impact of emergency medicine across the world.
Division of Global Emergency Medicine Team

Kristen Dettorre, MD
Division Director
Director, Global EM Fellowship
Associate Professor of Clinical Emergency Medicine

Assistant Professor of Emergency Medicine



